Current Research Grants
DoD AFIRM III (Armed Forces Institute for Regenerative Medicine): "Biofabrication of Surface-functionalized Composite Grafts for Vascularized Bone Regeneration Following Craniomaxillofacial Trauma", AFIRM Project MTF4. 2024-2028." (D. Dean, UWM Principal Investigator, Tony Atala, Wake Forest University)
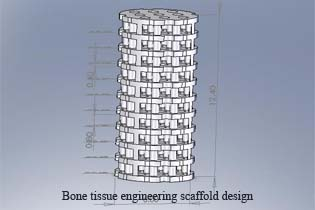
David Dean is the UW-Madison site PI; Tony Atala (Wake Forest Univ.) is the AFIRM directory. Abstract: We are using tethered ligands to functionalize bioprinted microvascular and 3D printed poly(propylene fumarate)-based bone tissue engineering scaffolds. We are using tethered ligands to avoid the non-specific release of dangerous cytokines, such as BMP2, into the patient. We are using chaotic printing to create thin membranes that encase rapidly branching arterioles and capillaries to supply of a 3D printed tissue-engineered bone graft at the point of implantation. We anticipate that this technology will become a standalone product simplifying tissue grafting procedures by providing an alternative to complex muscle grafts used to ensure perfusion of engrafted tissue. The chaotic printed vasculature is bolstered by a polymer fiber netting rendered via Melt Electrowriting (MEW). That netting is strong enough to provide suture retention and sufficient burst strength.
AFIRMNational Science Foundation (NSF) Engineering Research Center (ERC): "Autonomous Manufacturing: Manufacturing Evolution to Revolution (HAMMER). 2022-2027" (D. Dean is Lead, equiv. to Co-PI)
NSF HAMMER-ERC is developing a new approach to design and manufacturing, putting product needs first and then finding new manufacturing pathways based on the agility of artisans and reproducibility of machines. NSF HAMMER-ERC is the hub for technical, commercial, educational and standard setting for Hybrid Autonomous Manufacturing knowledge creation, deployment and commercial development.
NSF HAMMER ERCRecently Completed Research
Department of Defense Armed Forces Institute of Regenerative Medicine: W81XWH-14-2-0004: "Craniomaxillofacial Tissue Engineered Bone Grafts" (D. Dean, Project Leader)
The goal of this project is to develop a complete process to model, design, and generate implants to repair and improve outcomes following Craniomaxillofacial injury. The methods utilized in this project include 3D printing of resorbable implants that are precultured in a bioreactor using allogeneic bone progenitor cells. The precultured implant is placed in the defect site in order to draw in host tissue that will form bone of sufficient strength to bear dental implants. The project is working on the following specific aims in order to achieve these goals: Specific Aim 1: To determine the best use of the following data for tissue engineered implants that regenerate critical size maxillary and mandibular post-canine defects: (a) 3D CT images of the area to be repaired, (b) 3D surface templates of the area to be repaired and the surrounding CMF anatomy, (c) 3D printing PPF maxillary and mandibular implants, and (d) scaffold pore architecture that facilitates cell loading and scaffold resorption. Specific Aim 2: To determine the best means of promoting neobone formation in the implants designed in Aim 1 through: (a) bioreactor pre-culturing of bone marrow-derived MSCs, (b) facilitation of the vascularization of that neobone through proper care of the overlying periosteum and gingival tissue flap, and (c) determination of the pull-out strength of titanium dental posts implanted in the resulting maxillary and mandibular neobone. Specific Aim 3: To determine the protocol for a human clinical trial utilizing 3D printed PPF maxillary and mandibular implants, seeding those implants with (i.e., use of banked) cGMP human MSCs, and bioreactor culturing those implants to have a sufficient bone ECM coating to heal a critical size defect.
National Center for Regenerative Medicine: Demonstrator Project:"Mesenchymal Stem Cells (MSCs) for Tissue Engineered Bone Grafts" (D. Dean, Principal Investigator)
The goal of this project is to determine the best strategy to allow us to (a) receive a 3D CT scan from anywhere in the world, (b) plan the reconstructive surgical procedure, (c) where there was insufficient bone for transplantation in the patient’s body we could design a porous patient specific implant, (c) 3D print a porous resorbable scaffold for that patient, (d) use banked, MSCs to seed that scaffold, (e) preculture the MSC-seeded scaffold, and send a tissue-engineered bone graft to the prescribing surgeon for implantation. The project is an OH-Alive Demonstrator Project of the National Center for Regenerative Medicine's Ohio Alive Program. OH-Alive is a one-stop Stem Cell Innovator Platform that will enable for-profit entities, clinicians and academic researchers to better understand their cell culture protocols so that when they advance their cutting edge therapies from the bench to the bedside they can report to the FDA their manufacturing tolerances and sound scientific rationale for the methods they use in preparing their cell products. Ohio Alive's goals are: First, to transform medical therapy through the use of cells rather than drugs to heal tissues and organs. Second, to create the commercial and academic infrastructure in Ohio to establish a self-sufficient, vibrant biotechnology industry and support services that will attract cell therapy institutions across the US. (Information on “Ohio Alive” adapted from: http://ncrm.us/ohalive/landing.cfm)
 National Institutes of Health 5P01CA043892-18: Project 2: "Photodynamic Therapy - Basic Science Studies" (D. Dean, Co-Investigator)
National Institutes of Health 5P01CA043892-18: Project 2: "Photodynamic Therapy - Basic Science Studies" (D. Dean, Co-Investigator)
This Program Project will continue to investigate Photodynamic Therapy (PDT) as applied to solid tumor therapy. The clinical applications will focus on malignant brain tumors and prostate cancer. The four projects will cover research topics ranging from basic molecular and cellular responses to PDT to the conduct of novel clinical trials employing PDT. The projects are supported by two cores that are integral to the overall success of the Program. The synergy of the Program will continue to depend upon the effective interactions between both the scientific and clinical projects and the investigators. Project 1 will investigate in preclinical models novel strategies for the improved treatment of brain tumors. This project will incorporate aim one from prior Project 4 examining and comparing the molecular effects of ALA-mediated metronomic PDT versus acute ALA-mediated PDT in brain tumor. Project 2 consists of both ongoing and new clinical trials for the treatment of brain tumors. Project 3 will investigate in canine and murine models the possible use of PDT for the treatment of prostate tumors employing a novel, second-generation sensitizer, Tookad. Project 5 (not renumbered) will focus on the development of new biophysical techniques for monitoring PDT in vivo and on translating already developed methods and devices into clinical applications. Core 1 will provide the necessary administrative support for the overall Program and Core 2 will provide technical support to all of the preclinical and clinical projects.
National Institutes of Health: 5R01AR061460-02:"Application of tubular perfusion system (TPS) generated prevascularized bone tissue" (J. Fisher, Principal Investigator; D. Dean, Co-Investigator)
In vitro and in vivo nutrient transfer limits must be overcome in order to increase the feasibility of cell based therapeutic strategies. To enhance in vitro nutrient transport, the tubular perfusion system (TPS), a novel bioreactor recently developed by our laboratory, will dynamically culture human mesenchymal stem cells (hMSCs) in three dimensional scaffolds. This system utilizes an elegant design to create an effective cell culture environment without the drawbacks often associated with more complicated perfusion systems. The TPS design consists of hMSCs encapsulated in alginate beads which are tightly packed in a tubular growth chamber. Perfusing media through this growth chamber enhances nutrient transfer while exposing the cells to shear stress. To enhance in vivo vascularization, a prevascular network will be templated within the engineered tissue prior to implantation. To accomplish this, the TPS bioreactor will be optimized to support a coculture of endothelial cells and hMSCs. To examine this strategy of enhanced in vitro nutrient transport and in vivo vascularization, we propose first to investigate the TPS culture environment, particularly alginate bead size, bead composition, and media perfusion rate, that promotes hMSC proliferation and subsequent osteoblastic differentiation. Second, we propose to investigate the impact of endothelial cell coculture parameters, specifically coculture ratio, on the development of a prevascular network as well as the proliferation and differentiation of hMSCs. Third, we propose to implement a synthetic polymer sleeve system to support successful implantation of the in vitro cultured tissue. This strategy allows for the in vitro culture of functional engineered tissue, provides an elegant method for the in vivo implantation of the tissue, and fosters rapid integration of the implanted tissue into the host vasculature. Successful completion of these studies will demonstrate the feasibility of this fundamental technology for enhanced in vitro and in vivo nutrient transfer within cell based devices.
 National Institutes of Health: 2R01DE013740-06A1:"Strength and Resorption of Biodegradable Skull Implants" (D. Dean, Principal Investigator)
National Institutes of Health: 2R01DE013740-06A1:"Strength and Resorption of Biodegradable Skull Implants" (D. Dean, Principal Investigator)
Large skull defects arise frequently following neurosurgery and craniofacial reconstructive surgery for trauma, cancer resection, and congenital deformity. Concerns over revascularization, aesthetics and fixation of the implant are magnified by the post-surgical need to protect the underlying brain from both trauma and infection. Tissue engineered bone replacements have been shown to ossify small skeletal defects with potential utility in fracture site repair, but currently, these materials do not effectively address skull defects large enough to require graft or prosthetic augmentation. We propose to: (1) use Stereolithographic (SLA) rendering (i.e., rapid prototyping) of poly(propylene fumarate)/b-tricalcium phosphate (PPF/b-TCP) to produce porous implants with computer-modeled mechanical, geometric, cell attachment (i.e., in vitro in a bioreactor, or in vivo), and resorption properties; (2) use a nude rat intra-muscular pocket (i.e., bone ossicle) model to test the in vivo interaction of PPF/b-TCP, canine osteoprogenitor cells, and growth factors; (3) select the best performing (i.e., rate and strength of bone produced) construct to elevate to a critical size (i.e., 2.5 cm) and then a super-critical size (i.e., 4.0 cm) canine cranial implant. In order to accomplish these goals we propose the following specific aims: (1) Determine an effective pore geometry and surface texture for cRBM and/or cMSC loading and seeding of SLA-rendered, porous PPF/b-TCP scaffolds. (2) Determine the most osteogenic combination of the best AIM 1 scaffolds (i.e., PPF geometry, PPF texture, cRBM, or cMSCs), bioreactor or in vivo cell culture, and autologous (platelets, cRBM) and/or exogenous (TGF-b2, BMP-2, BMP-7, FGF-2 and VEGF) growth factors in a nude rat intra-muscular bone ossicle model. Subaim: Determine whether pre-implantation bioreactor culturing improves rate and quality of bone formation. (3) Determine whether the best performing bone ossicle strategy for the nude rat produces reliable infilling of initially critical size (2.5 cm) circular, biparietal, cranial implants in the dog. A second cycle of Aims 1-3 in years 4-5 will use what is learned in Cycle I to maximally expand the area of reliably grown bone from 2.5 to 4.0 cm or larger. Unlike current standard of care PMMA and titanium cranial implants, reliable resorption and bone formation in PPF/b-TCP scaffolds will serve to seal off the cranial cavity from infection, better translate traumatic stress to the rest of the skull, and remodel with the rest of the skull over time.
State of Ohio Third Frontier:"Clinical Tissue Engineering Center", Project 4: "Rapid Fabrication of BioScaffolds with Light Polymerizeable Polymers" (D. Dean, Co-Investigator)
Project 4: Aim: To assess the efficacy of stereolithographic (SLA) 3D printing (i.e., rapid prototyping) of biodegradable implants. Abstract: The complex geometry of cranial bone defects presents a serious surgical challenge. Preoperative fabrication of implants that match the defect geometry greatly improves fixation and the cosmetic result. Dr. Dean has developed software to design patient-specific implants from 3D CT scans that can then be rendered using a stereolithographic (SLA) prototyping device. Dr. Dean and others have patented a new STL method for direct production of impants via the photo-polymerization of (poly)propylene fumarate (PPF) or other resorbable polymers. This project seeks to establish the efficacy and commercial potential for the rapid prototyping of light polymerizable tissue engineering scaffold materials.